Appendicitis (or epityphlitis) is a condition characterized by inflammation of the appendix. All cases require removal of the inflamed appendix, either by laparotomy or laparoscopy. Untreated, mortality is high, mainly because of peritonitis and shock.[1] Reginald Fitz first described acute appendicitis in 1886,[2] and it has been recognized as one of the most common causes of severe acute abdominal pain worldwide.
Causes of Appendicitis
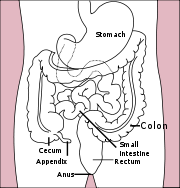 Location of the appendix in the digestive system
Location of the appendix in the digestive system
On the basis of experimental evidence, acute appendicitis seems to be the end result of a primary obstruction of the appendix lumen.[3][4] Once this obstruction occurs the appendix subsequently becomes filled with mucus and swells, increasing pressures within the lumen and the walls of the appendix, resulting in thrombosis and occlusion of the small vessels, and stasis of lymphatic flow. Rarely, spontaneous recovery can occur at this point. As the former progresses, the appendix becomes ischemic and then necrotic. As bacteria begin to leak out through the dying walls, pus forms within and around the appendix (suppuration). The end result of this cascade is appendiceal rupture causing peritonitis, which may lead to septicemia and eventually death.
Among the causative agents, such as foreign bodies, trauma, intestinal worms, and lymphadenitis, the occurrence of an obstructing fecalith has attracted attention. The prevalence of fecaliths in patients with appendicitis is significantly higher in developed than in developing countries[5], and an appendiceal fecalith is commonly associated with complicated appendicitis[6]. Also, fecal stasis and arrest may play a role, as demonstrated by a significantly lower number of bowel movements per week in patients with acute appendicitis compared with healthy controls[7]. The occurrence of a fecalith in the appendix seems to be attributed to a right sided fecal retention reservoir in the colon and a prolonged transit time[8]. From epidemiological data it has been stated that diverticular disease and adenomatous polyps were unknown and colon cancer exceedingly rare in communities exempt for appendicitis[9][10]. Also, acute appendicitis has been shown to occur antecedent to cancer in the colon and rectum[11]. Several studies offer evidence that a low fiber intake is involved in the pathogenesis of appendicitis[12] [13][14]. This is in accordance with the occurrence of a right sided fecal reservoir and the fact that dietary fiber reduces transit time[15].
Symptoms of Appendicitis
Symptoms of acute appendicitis can be classified into two types, typical and atypical.[1] The typical history includes pain starting centrally (periumbilical) before localizing to the right iliac fossa (the lower right side of the abdomen); this is due to the poor localizing (spatial) property of visceral nerves from the mid-gut, followed by the involvement of somatic nerves (parietal peritoneum) as the inflammation progresses. The pain is usually associated with loss of appetite and fever, although the latter isn’t a necessary symptom. Nausea or vomiting may occur, and also the feeling of drowsiness and the feeling of general bad health. With the typical type, diagnosis is easier to make, surgery occurs earlier and findings are often less severe.[1]
Atypical symptoms may include pain beginning and staying in the right iliac fossa, diarrhea and a more prolonged, smoldering course. If an inflamed appendix lies in contact with the bladder, there is frequency of micturition. With post-ileal appendix, marked retching may occur. Tenesmus or “downward urge” (the feeling that a bowel movement will relieve discomfort) is also experienced in some cases.[16]
Signs
These include localized findings in the right iliac fossa. The abdominal wall becomes very sensitive to gentle pressure (palpation). Also, there is rebound tenderness. In case of a retrocecal appendix, however, even deep pressure in the right lower quadrant may fail to elicit tenderness (silent appendix), the reason being that the cecum, distended with gas, prevents the pressure exerted by the palpating hand from reaching the inflamed appendix. Similarly, if the appendix lies entirely within the pelvis, there is usually complete absence of the abdominal rigidity. In such cases, a digital rectal examination elicits tenderness in the rectovesical pouch. Coughing causes point tenderness in this area (McBurney’s point) and this is the least painful way to localize the inflamed appendix. If the abdomen on palpation is also involuntarily guarded (rigid), there should be a strong suspicion of peritonitis requiring urgent surgical intervention.
Other signs are:
Rovsing’s sign
Deep palpation of the left iliac fossa may cause pain in the right iliac fossa. This is the Rovsing’s sign, also known as the Rovsing’s symptom. It is used in the diagnosis of acute appendicitis. Pressure over the descending colon causes pain in the right lower quadrant of the abdomen.[17]
Psoas sign
Occasionally, an inflamed appendix lies on the psoas muscle and the patient will lie with the right hip flexed for pain relief.
Obturator sign
If an inflamed appendix is in contact with the obturator internus, spasm of the muscle can be demonstrated by flexing and internally rotating the hip. This Maneuver will cause pain in the hypogastrium.
Investigations of Appendicitis
Diagnosis is based on patient history (symptoms) and physical examination backed by an elevation of neutrophilic white blood cells. Atypical histories often require imaging with ultrasound and/or CT scanning.[1] A pregnancy test is vital in all women of child bearing age, as ectopic pregnancies and appendicitis present with similar symptoms. The consequences of missing an ecoptic pregnancy are serious, and potentially life threatening. Furthermore the general principles of approaching abdominal pain in women (in so much that it is different from the approach in men) should be appreciated.
Ultrasonography and Doppler sonography provide useful means to detect appendicitis, especially in children. In some cases (15% approximately), however, ultrasonography of the iliac fossa does not reveal any abnormalities despite the presence of appendicitis. This is especially true of early appendicitis before the appendix has become significantly distended and in adults where larger amounts of fat and bowel gas make actually seeing the appendix technically difficult. Despite these limitations, in experienced hands sonographic imaging can often distinguish between appendicitis and other diseases with very similar symptoms such as inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or fallopian tubes.
In places where it is readily available, CT scan has become the diagnostic test of choice, especially in adults whose diagnosis is not obvious on history and physical. (The use of CT in pregnant women and children is significantly limited, however, by concerns regarding radiation exposure.) A properly performed CT scan with modern equipment has a detection rate (sensitivity) of over 95% and a similar specificity. Signs of appendicitis on CT scan include lack of oral contrast (oral dye) in the appendix, direct visualization of appendiceal enlargement (greater than 6 mm in diameter on cross section), and appendiceal wall enhancement (IV dye). The inflammation caused by appendicitis in the surrounding peritoneal fat (so called “fat stranding”) can also be observed on CT, providing a mechanism to detect early appendicitis and a clue that appendicitis may be present even when the appendix is not well seen. Thus, diagnosis of appendicitis by CT is made more difficult in very thin patients and in children, both of whom tend to lack significant fat within the abdomen. The utility of CT scanning is made clear, however, by the impact it has had on negative appendectomy rates. For example, use of CT for diagnosis of appendicitis in Boston, MA has decreased the chance of finding a normal appendix at surgery from 20% in the pre-CT era to only 3% according to data from the Massachusetts General Hospital.
According to a systematic review from UC-San Francisco comparing ultrasound vs. CT scan, CT scan is more accurate than ultrasound for the diagnosis of appendicitis in adults and adolescents. CT scan has a sensitivity of 94%, specificity of 95%, a positive likelihood ratio of 13.3 (CI, 9.9 to 17.9), and a negative likelihood ratio of 0.09 (CI, 0.07 to 0.12). Ultrasonography had an overall sensitivity of 86%, a specificity of 81%, a positive likelihood ratio of 5.8 (CI, 3.5 to 9.5), and a negative likelihood ratio of 0.19 (CI, 0.13 to 0.27).[18]
Matrix metalloproteinase (MMP) levels can be used as biomarkers of increased risk of appendiceal rupture among patients with acute appendicitis according to a cohort study.[19] MMP-1 was higher in gangrenous (p<0.05) and perforated appendicitis (p<0.01) compared with controls. MMP-9 was most abundantly expressed in inflamed appendix and reached a tenfold higher expression in all groups with appendicitis compared with controls (p<0.001).
A number of clinical and laboratory based scoring systems have been devised to assist diagnosis. The most widely used is Alvarado score.
Alvarado score
| Symptoms | |
|---|---|
| Migratory right iliac fossa pain | 1 point |
| Anorexia | 1 point |
| Nausea and vomiting | 1 point |
| Signs | |
| Right iliac fossa tenderness | 2 points |
| Rebound tenderness | 1 point |
| Fever | 1 point |
| Laboratory | |
| Leucocytosis | 2 points |
| Shift to left (segmented neutrophils) | 1 point |
| Total score | 10 points |
A score of 7 or more is strongly predictive of acute appendicitis.
In patients with an equivocal score of 5-6, CT scan further reduces the rate of negative appendicectomy.
Treatment of Appendicitis
The treatment begins by keeping the patient from eating or drinking anything, even water, in preparation for surgery. An intravenous drip is used to hydrate the patient. Antibiotics given intravenously such as cefuroxime and metronidazole may be administered early to help kill bacteria and thus reduce the spread of infection in the abdomen and postoperative complications in the abdomen or wound. Equivocal cases may become more difficult to assess with antibiotic treatment and benefit from serial examinations. If the stomach is empty (no food in the past six hours) general anaesthesia is usually used. Otherwise, spinal anaesthesia may be used.
The surgical procedure for the removal of the appendix is called an appendicectomy (also known as an appendectomy). Often now the operation can be performed via a laparoscopic approach, or via three small incisions with a camera to visualize the area of interest in the abdomen. If the findings reveal suppurative appendicitis with complications such as rupture, abscess, adhesions, etc., conversion to open laparotomy may be necessary. An open laparotomy incision if required most often centers on the area of maximum tenderness, McBurney’s point, in the right lower quadrant. A transverse or a gridiron diagonal incision is used most commonly.
In March 2008, an American woman had her appendix removed via her vagina, in a medical first.[20]
According to a meta-analysis from the Cochrane Collaboration comparing laparoscopic and open procedures, laparoscopic procedures seem to have various advantages over the open procedure. Wound infections were less likely after laparoscopic appendicectomy than after open appendicectomy (odds ratio 0.45; CI 0.35 to 0.58), but the incidence of intraabdominal abscesses was increased (odds ratio 2.48; CI 1.45 to 4.21). The duration of surgery was 12 minutes (CI 7 to 16) longer for laparoscopic procedures. Pain on day 1 after surgery was reduced after laparoscopic procedures by 9 mm (CI 5 to 13 mm) on a 100 mm visual analogue scale. Hospital stay was shortened by 1.1 day (CI 0.6 to 1.5). Return to normal activity, work, and sport occurred earlier after laparoscopic procedures than after open procedures. While the operation costs of laparoscopic procedures were significantly higher, the costs outside hospital were reduced. Young female, obese, and employed patients seem to benefit from the laparoscopic procedure more than other groups. [21]
There is debate whether emergent appendicectomy (within 6 hours of admission) reduces the risk of perforation or complication versus urgent appendicectomy (greater than 6 hours after admission). According to a retrospective case review study [22] no significant differences in perforation rate among the two groups were noted (P=.397). Various complications (abscess formation, re-admission) showed no significant differences (P=0.667, 0.999). According to this study, beginning antibiotic therapy and delaying appendicectomy from the middle of the night to the next day does not significantly increase the risk of perforation or other complications. These findings may fit a theory that acute (typical) appendicitis and suppurative (atypical) appendicitis are two distinct disease processes. Findings at the time of surgery suggest that perforation occurs at the onset of symptoms in atypical cases.(1)
Surgery may last from 15 minutes in typical appendicitis in thin patients to several hours in complicated cases. Hospital lengths of stay usually range from overnight to a matter of days (rarely weeks in complicated cases.) The pain is not always constant; in some cases it can stop for a day and then come back.
Differential diagnosis
In children:
- Gastroenteritis, mesenteric adenitis, Meckel’s diverticulitis, intussusception, Henoch-Schönlein purpura, lobar pneumonia
In adults:
- regional enteritis, renal colic, perforated peptic ulcer, testicular torsion, pancreatitis, rectus sheath hematoma, pelvic inflammatory disease, ectopic pregnancy, endometriosis, torsion/rupture of ovarian cyst
In elderly:
- diverticulitis, intestinal obstruction, colonic carcinoma, mesenteric ischemia, leaking aortic aneurysm.
Prognosis
Most appendicitis patients recover easily with surgical treatment, but complications can occur if treatment is delayed or if peritonitis occurs. Recovery time depends on age, condition, complications, and other circumstances, including the amount of alcohol consumption, but usually is between 10 and 28 days. For young children (around 10 years old) the recovery takes three weeks.
The real possibility of life-threatening peritonitis is the reason why acute appendicitis warrants speedy evaluation and treatment. The patient may have to undergo a medical evacuation. Appendectomies have occasionally been performed in emergency conditions (i.e. outside of a proper hospital), when a timely medical evaluation was impossible.
Typical acute appendicitis responds quickly to appendectomy and occasionally will resolve spontaneously. If appendicitis resolves spontaneously, it remains controversial whether an elective interval appendectomy should be performed to prevent a recurrent episode of appendicitis. Atypical appendicitis (associated with suppurative appendicitis) is more difficult to diagnose and is more apt to be complicated even when operated early. In either condition prompt diagnosis and appendectomy yield the best results with full recovery in two to four weeks usually. Mortality and severe complications are unusual but do occur, especially if peritonitis persists and is untreated. Another entity known as appendicular lump is talked about quite often. It happens when appendix is not removed early during infection and omentum and intestine get adherent to it forming a palpable lump. During this period operation is risky unless there is pus formation evident by fever and toxicity or by USG. Medical management treats the condition.
An unusual complication of an appendectomy is “stump appendicitis”: inflammation occurs in the remnant appendiceal stump left after a prior, incomplete appendectomy.[23]
Homeopathy Treatment for Appendicitis
Keywords: homeopathy, homeopathic, treatment, cure, remedy, remedies, medicine
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc. A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’. The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy. To study any of the following remedies in more detail, please visit the Materia Medica section at www.kaisrani.com.
None of these medicines should be taken without professional advice and guidance.
Homeopathy Remedies for Appendicitis :
Bell., bry., cadm-s., calc-s., chin., chel., cocc., coloc., con., crot-c., dulc., echi., graph., hep., ign., iris-t., lach., lyc., merc., merc-c., nit-ac., phos., plb., sil., ter.
References
- ^ a b c d Hobler, K. (Spring 1998). “Acute and Suppurative Appendicitis: Disease Duration and its Implications for Quality Improvement“. Permanente Medical Journal 2 (2), http://xnet.kp.org/permanentejournal/spring98pj/Spring98.pdf#page=7.
- ^ Fitz RH (1886). “Perforating inflammation of the vermiform appendix with special reference to its early diagnosis and treatment”. Am J Med Sci (92): 321–46.
- ^ Wangensteen OH, Bowers WF (1937). “Significance of the obstructive factor in the genesis of acute appendicitis”. Arch Surg 34: 496-526.
- ^ Pieper R, Kager L, Tidefeldt U (1982). “Obstruction of appendix vermiformis causing acute appendicitis. An experimental study in the rabbit”. Acta Chir Scand 148 (1): 63–72. PMID 7136413.
- ^ Jones BA, Demetriades D, Segal I, Burkitt DP (1985). “The prevalence of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa“. Ann. Surg. 202 (1): 80–2. PMID 2990360.
- ^ Nitecki S, Karmeli R, Sarr MG (1990). “Appendiceal calculi and fecaliths as indications for appendectomy”. Surg Gynecol Obstet 171 (3): 185–8. PMID 2385810.
- ^ Arnbjörnsson E (1985). “Acute appendicitis related to faecal stasis”. Ann Chir Gynaecol 74 (2): 90–3. PMID 2992354.
- ^ Raahave D, Christensen E, Moeller H, Kirkeby LT, Loud FB, Knudsen LL (2007). “Origin of acute appendicitis: fecal retention in colonic reservoirs: a case control study”. Surg Infect (Larchmt) 8 (1): 55–62. doi:10.1089/sur.2005.04250. PMID 17381397.
- ^ Burkitt DP (1971). “The aetiology of appendicitis”. Br J Surg 58 (9): 695–9. PMID 4937032.
- ^ Segal I, Walker AR (1982). “Diverticular disease in urban Africans in South Africa”. Digestion 24 (1): 42–6. PMID 6813167.
- ^ Arnbjörnsson E (1982). “Acute appendicitis as a sign of a colorectal carcinoma”. J Surg Oncol 20 (1): 17–20. PMID 7078180.
- ^ Burkitt DP, Walker AR, Painter NS (1972). “Effect of dietary fibre on stools and the transit-times, and its role in the causation of disease”. Lancet 2 (7792): 1408–12. PMID 4118696.
- ^ Adamis D, Roma-Giannikou E, Karamolegou K (2000). “Fiber intake and childhood appendicitis”. Int J Food Sci Nutr 51: 153–7.
- ^ Hugh TB, Hugh TJ (2001). “Appendicectomy–becoming a rare event?“. Med. J. Aust. 175 (1): 7–8. PMID 11476215, http://www.mja.com.au/public/issues/175_01_020701/hugh/hugh.html.
- ^ Gear JS, Brodribb AJ, Ware A, Mann JI (1981). “Fibre and bowel transit times“. Br. J. Nutr. 45 (1): 77–82. PMID 6258626, http://journals.cambridge.org/abstract_S0007114581000111.
- ^ http://digestive.niddk.nih.gov/ddiseases/pubs/appendicitis/#1 National Digestive Diseases Information Clearinghouse (NDDIC)
- ^ N. T. Rovsing: Indirektes Hervorrufen des typischen Schmerzes an McBurney’s Punkt. Ein Beitrag zur diagnostik der Appendicitis und Typhlitis. Zentralblatt für Chirurgie, Leipzig, 1907, 34: 1257-1259.
- ^ Terasawa T, Blackmore CC, Bent S, Kohlwes RJ (2004). “Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents”. Ann. Intern. Med. 141 (7): 537–46. PMID 15466771.
- ^ Solberg A, Holmdahl L, Falk P, Palmgren I, Ivarsson ML (2008). “A local imbalance between MMP and TIMP may have an implication on the severity and course of appendicitis”. Int J Colorectal Dis 23: 611. doi:10.1007/s00384-008-0452-x. PMID 18347803.
- ^ Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Prasad M (March 2008). “Transvaginal endoscopic appendectomy in humans: a unique approach to NOTES-world’s first report”. Surg Endosc. doi:10.1007/s00464-008-9811-5. PMID 18347865. ScienceDaily report
- ^ Sauerland S, Lefering R, Neugebauer EA (2004). “Laparoscopic versus open surgery for suspected appendicitis”. Cochrane Database Syst Rev (4): CD001546. doi:10.1002/14651858.CD001546.pub2. PMID 15495014.
- ^ Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG (2004). “Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night?”. J. Pediatr. Surg. 39 (3): 464–9; discussion 464–9. doi:10.1016/j.jpedsurg.2003.11.020. PMID 15017571.
- ^ Liang MK, Lo HG, Marks JL (2006). “Stump appendicitis: a comprehensive review of literature”. The American surgeon 72 (2): 162–6. PMID 16536249.
Related posts:
